MEDICAID COVERAGE MANAGEMENT
Provide Your Patients with Coverage Management
Medicaid patients deserve to know that you're there for them. Be there, with PointCare.
LAPSE DETECTION
Monitors the patient's Medicaid status, checking to see if they've lost coverage and need to take action.
PATIENT OUTREACH
Patients receive text messages, emails, and phone calls, letting them know they've lost coverage and to reapply.
ONLINE ENROLLMENT
Patients receive a link to our online enrollment platform, which quickly walks them through the enrollment process.
APPLICATION SUBMISSION
Completed Medicaid applications are submitted directly to the state's Medicaid office, and processed on patients' behalf.
SELF-PAY CONVERSION
Engages patients that are qualified and without coverage, enrolling them in Medicaid.
REVENUE RESCUE
Automatically monitors self-pay encounters and notifies you if they are eligible for Medicaid reimbursement.
Ready to Improve your Patients' Lives?
SCHEDULE A CALL
Let's discuss the challenges you're facing and work together to develop the best solution for you and your patients.
Provide your Patients Easy and Convenient
Online Medicaid Enrollment
- Expand your enrollment team
- Provide a secure online enrollment environment
- Can be used by patients & enrollment teams
- Submits Medicaid applications directly to Medicaid on patients' behalf
REVENUE RESCUE
Combines retroactive revenue recovery, and the proactive power of PointCare, with zero contingency fees.1
Upload
Upload a list of your recent uncovered & self-pay encounters.
2
Monitor
We monitor your patients to see if they've gained Medicaid coverage, enabling reimbursement.
3
Outreach
We reach out to your uncovered patients, getting them enrolled in Medicaid.
4
Manage
Once a patient is covered, we manage their coverage and notify them if they lose coverage.
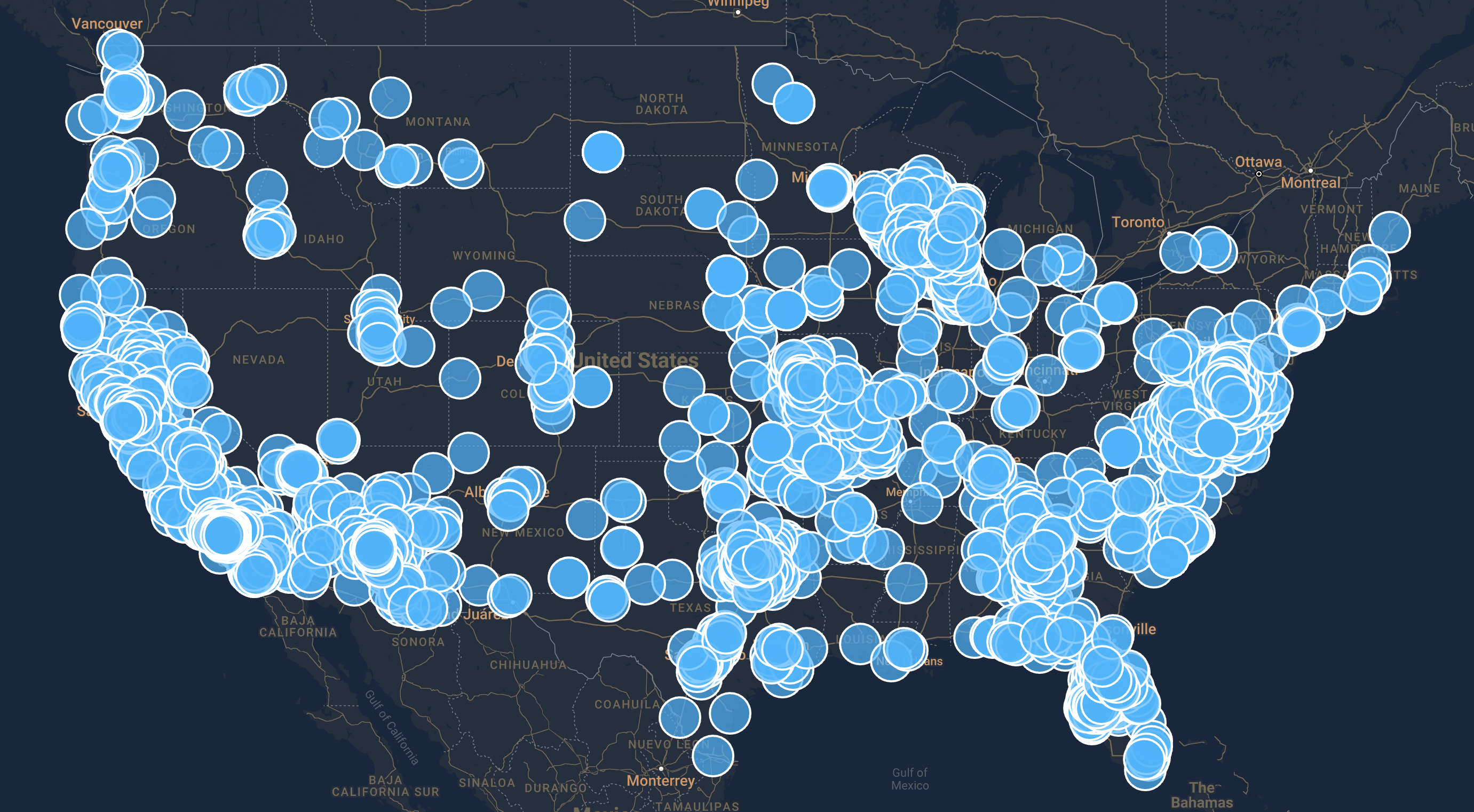
Managing Coverage for 3M+ Medicaid Patients