IT'S ALMOST 2025, IT'S TIME TO . . .
Provide Your Patients with Coverage Management
Medicaid patients deserve to know that you're there for them. Be there, with PointCare.
LAPSE DETECTION
Our service detects when your patients lose their Medicaid coverage.
PATIENT OUTREACH
We text, call and email patients to assist with their Medicaid re-enrollment.
ONLINE ENROLLMENT
We provide a secure and intuitive way for your patients to submit applications.
Ready to Improve your Patients' Lives?
SCHEDULE A CALL
Our Medicaid experts will help identify your challenges and craft the best service solution for you and your patients.
.png?width=300&name=Com%20Headshots%20(17).png)
TOUCH
Alex Richmond
Director of FQHC Partnerships
.png?width=300&name=Com%20Headshots%20(16).png)
TOUCH
Marisa Williams
Sr. Account Executive
AZ•AR•CO•IL•IN•IA•KS•LA•MI•MN
•MO•NE•ND•OH•OK•SD•TX•UT
•WI•WY
Schedule a Call
Marisa Williams
Sr. Account Executive
-1.png?width=300&name=Com%20Headshots%20(13)-1.png)
TOUCH
Julian Graham
SR. Account Executive
AL•CT•DE•DC•FL•GA•KY•ME
•MD•MA•MS•NH•NJ•NY•NC•PA
•RI•SC•TN•VT•VA•WV
Julian Graham
SR. Account Executive
Provide your Patients Easy and Convenient
Online Medicaid Enrollment
- Expand your enrollment team
- Provide a secure online enrollment environment
- Can be used by patients & enrollment teams
- Submits Medicaid applications directly to Medicaid on patients' behalf
RETRO DETECTION
Combines retroactive revenue recovery, and the proactive power of PointCare, with zero contingency fees.1
Upload
Upload a list of your recent uncovered & self-pay encounters.
2
Monitor
We monitor your patients to see if they've gained Medicaid coverage, enabling reimbursement.
3
Outreach
We reach out to your uncovered patients, getting them enrolled in Medicaid.
4
Manage
Once a patient is covered, we manage their coverage and notify them if they lose coverage.
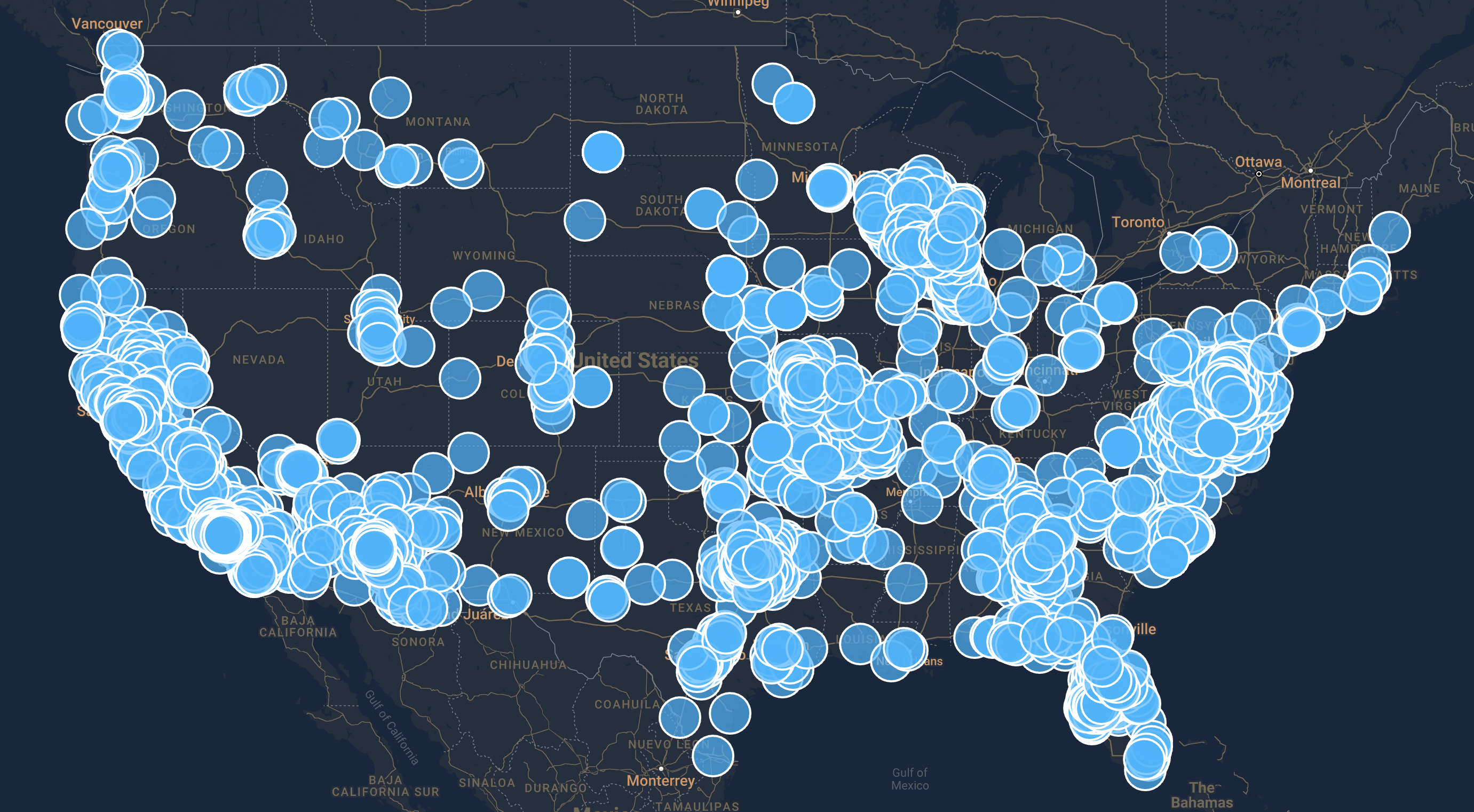
Managing Coverage for 3M+ Medicaid Patients